Lung cancer is the scourge of our time. There is almost no family who does not have an incident either in the surroundings or within the same as it has not been diagnosed with lung cancer. Unfortunately, news from local and international news show only cases of lung cancer that eventually failed.
What’s wrong? Is it an immovable cancer or is there hope and can we win it?
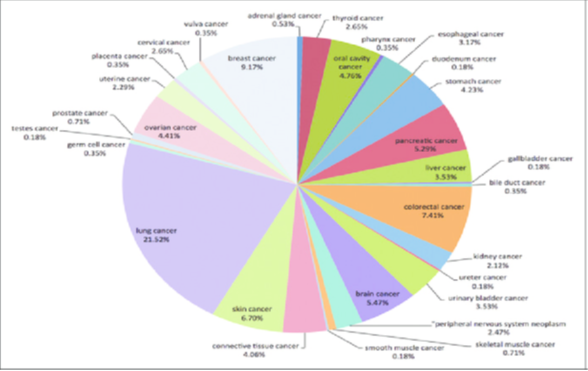
Lung cancer is the most common cause of cancer worldwide. Nearly 22%, that is, 1 in the 5 cancers diagnosed today are lung cancer when the second cause is breast with only 9%, in short, lung cancer is more than twice the appearance of the second form of cancer worldwide.
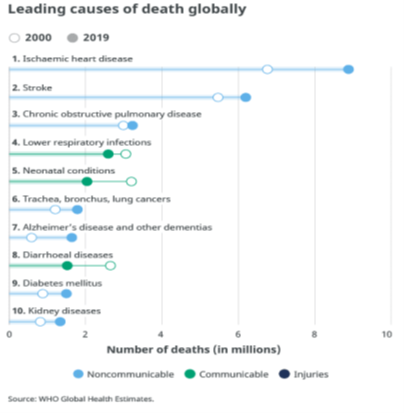
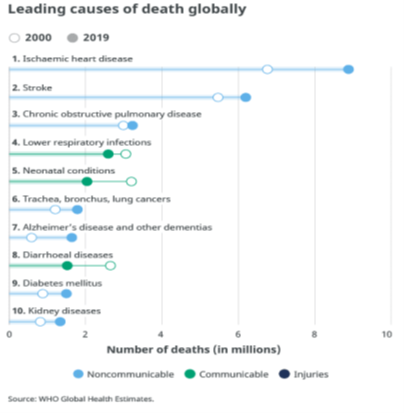
According to WHO (Figure No. 2) lung cancer alone as an entity is the 6th cause of death worldwide. So we understand what we are talking about.
But where is the poor survival and why does it really seem to be invulnerable?
The main reason is that with the exception of a small percentage of case that occur centrally, that is, in a large airway (mainly loop), all other cases relate to peripheral masses that do not give symptoms. Therefore, when the patient has these first symptoms are not from cancer but usually from his metastases and so things are difficult.
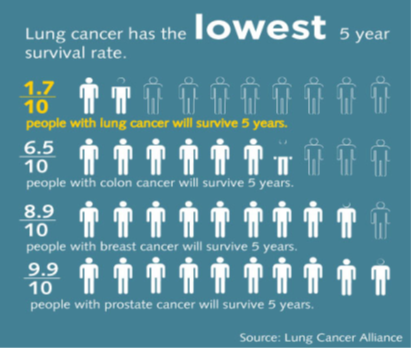
There is a huge reason for prevention as it is a cancer that is largely associated with smoking. Just as important, perhaps even more important to me, but it is early diagnosis because, as I will analyze below, if this cancer is diagnosed at an early stage then after surgical exception we can talk about IASA! That is, we can beat the worst cancer that exists right now and plagues humanity.
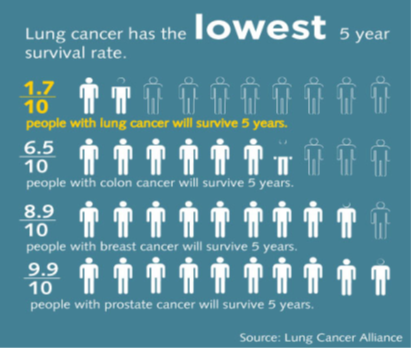
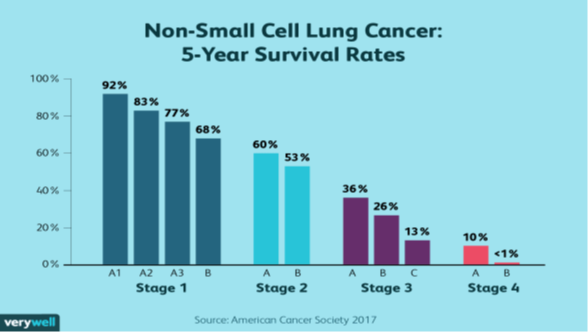
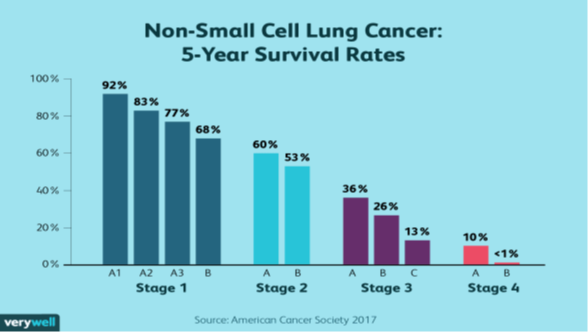
The development of a patient with lung cancer is prescribed and depends on the stage the patient is classified at the time of the diagnosis. As shown in the table below there are essentially four stages with various subcategories. Consequently, the earlier a lung cancer is found and treated, that is, the closer we are to Stage 1, the complete healing is the rule, not the exception. On the contrary, the closer we are to stage 4 then the case of healing is literally zero.
So how can we have hopes of winning it from the time we find a lung cancer early?
Here all scientists dealing with lung cancer agree that in order for the patient to have hopes and if he is initial stage he must undergo surgery. After the intervention both some details associated with it (eg size) and some important elements to be taken into account, such as the condition of the lymph nodes (filtered or not), will classify the patient at a post -operative stage, which is and what counts. That is, it can be another imaging stage (from axial and Ret) and another the real stage of the patient. So the smaller the stage at which the patient will eventually find, the more likely it is to be saved than to end up with cancer and the smaller the stage the patient does not need further complementary treatment (chemotherapy, radiotherapy).
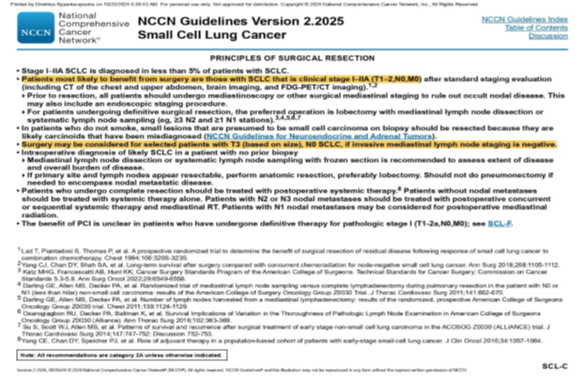
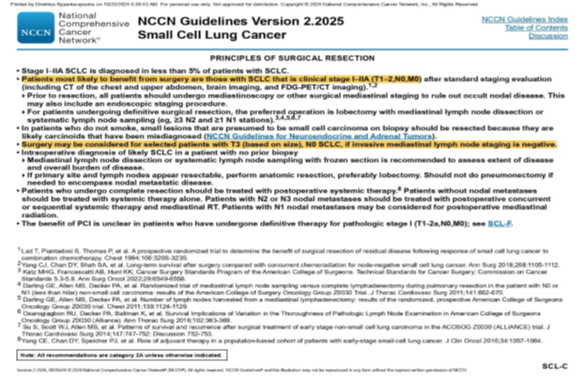
So, having understood the importance of early diagnosis we need to see when this is achieved what the patient’s choices are. As we said before if the word surgery does not enter the equation, the patient has almost no chance of being canceled by his cancer. Even types of cancer that were once considered to be unmistakable, such as microcycaneal lung cancer, now with the latest data (NCCN Guidelines) can be operated up to Stage IIB.
Since the patient is judged, after pre -operative control, that he is a candidate for surgery, the ideal procedure to undergo depends solely on the thoracic surgeon who of course has experience and many years of proven action on the operating table. Ideally a patient should undergo a lobectomy if the damage involves a lobe of his lung. By lobe we mean an anatomical portion of the lung, which for history, we have two lungs, one right and one left, in which the left has two pieces, the up and down, that is, two lobes, while the right lung has three lobes: the upper one. So if the cancer is found, for example, in the upper lobe of the right lung, then the patient should ideally undergo a lobe lobe lobe, that is, the part of that lung containing cancer alone. If the cancer catches two parts of the lung, for example, the upper and the average lobe then it must be subjected to dulweal, that is, the removal of both the upper and the average lobe or if it catches the three lobes right or the two left then the patient may be subjected to one.
Whether it will be able to survive after such a large and demanding surgery depends naturally both on the patient’s physical condition but mainly on a test performed in pre -operative control and showing us how much of the lung is allowed to remove in the surgery. This test, spirometry, may need to be combined with other more specialized tests such as diffusion or a ventilation/haemmorization test when we need to receive more information that may force us to modify our original plan for the surgery.
Pneumonectomy should be avoided and there are various techniques that we can replace with a lobectomy as long as there is a thoracic surgeon experience. The main reason this is that we do not want to leave the patient almost with a disability but also because pneumonectomy has twice as much mortality from lobectomy that reaches 8-10% when the mortality of lobectomy is about 5% and when the mortality for about 1% is about 1%.
If a patient is considered marginal and we are not so sure of whether he will be able to cope after surgery, but the need for surgery is huge because otherwise he has no hope of living, we sometimes have to think alternatively and make some “discounts”. These are none other than some modified procedures, instead of lobectomy, such as section or wedge resection. There is a great deal of debate today about the results of these interventions compared to lobectomy that in many cases seem to be similar, although my personal view is that lobectomy is superior to all of them.
So let’s assume that we have a patient who has been diagnosed with lung cancer and fortunately is at premature stage and so it can be operated on.
What are the therapeutic surgical choices he has?
Surgical chest has many weapons in their quiver and the specialty, as well as most specialties in medicine over the years, has progressed. Thus, from the “outdated” chests where we had to cut between the sides and break parts of them to access the anatomical points of the lung we had to remove, at the end of the 90s the thoracic interventions were resulted in the An experienced and trained surgeon performs the same operation as he would openly handle a 30-40cm cut, from a incision that does not exceed 4cm.
The further development of the surgical chest came after the revolution of the appearance of the Da Vinci robotic system and its adoption by the thoracic surgeons. Interventions are now being done almost without the existence of incisions, with much greater security for both the patient and the doctor naturally and practically today there is no operation that cannot be done with the use of Robot. Understand the range of surgery now covered, recently a robotic lung transplant has been carried out for the first time in medical time!
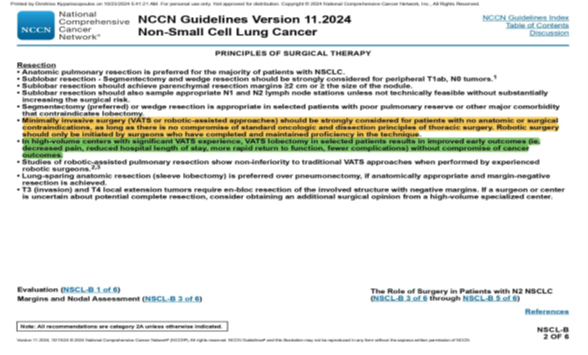
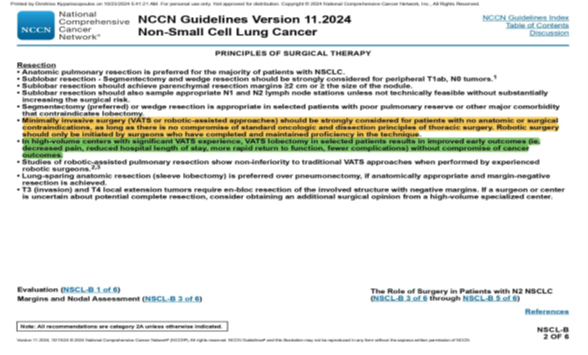
As a professor of robotic surgery but also as a thoracic surgeon who performs the entire range of procedures, it is clear that since there is no anatomical problem I prefer robotic surgery for my patients. This is not my view but also an international guideline (NCCN Guidelines) (Figure 6) urging surgeons to only surgery in a minimally invasive way, namely thoracic or robotics, as it has been shown that patients who are in this way have better prognosis.
Being the director of the clinic that performs the largest number of robotic interventions in Greece and Cyprus, at the moment, the results after a robotic lobectomy are not capable of questioning. The overwhelming majority of our patients are discharged 24 hours after surgery and almost all within 48 hours. There is no patient who when he woke up to know where his incision is and hurts in the surgical holes we used to get the robotic tools.
With so fast and rapid recovery but mainly with extremely oncological results as the help provided by Robot da Vinci both to the handling of its arms and tools and in the huge enlargement, which sometimes reaches all 20 times, allows us to avoid mistakes but also to distinguish the anatomic variations, Scientific community and now in all civilized states, robotic treatment of lung cancer is the first choice. We are not only saying this, but also our patients themselves who present and share their experiences and are a guide to other patients who may be doubting which method is best for them.
Robotic surgery in treatment of lung cancer is now a conquest and we should never go back, on the contrary, more and more colleagues have to gain access and experience in handling it. Consequently, when we can be as a state, as a state and everyone, we can enter a regular control as there is, for example, in women with mammography or test Pap, and we can detect forms of lung cancer at premature stage then the mortality rates will fall dramatically. So, although more cases will occur, more patients who have been diagnosed with lung cancer will survive, and as I say to my own patients who come to operate them, they will die for a while than they want but not from lung cancer!


Professor MR Dimitrios Kyparissopoulos
Thoracic surgeon, MD, MD PHSC, FRCS EA
Robotics and thoracoscopic minimally invasive surgery
Professor of Robotic Surgery, Medical School of European University
Director of the Thoracic Surgery of IASO Athens Clinic
Honorary Hospital Curator Harefield, Royal Brompton and Harefield NHS Foundation Trust, London, UK
Former Harefield Hospital Hospital Curator Hospital, London, UK
Former Hospital Curator JR, Oxford University Hospital, UK
Specialized thoracic surgeon
